QuNaMai Urogynecological Plasma Surgical System
Author: QuNaMai
Release time: 2025-09-03 18:02:46
View number: 451
QuNaMai Urogynecological Plasma Surgical System
Host: Hey everyone, welcome back to "Medical Tech Insights"—your go-to spot for breaking down game-changing tools that make healthcare safer and more efficient. Today, we’re diving into a product that’s turning heads in both urology and gynecology: the QuNaMai Plasma Surgical System. I’m joined by Dr. Elena Carter, a product specialist with deep expertise in minimally invasive surgical devices. Elena, thanks for being here!
Dr. Carter: Thanks for having me! I’m excited to talk about this system—It’s not just another piece of equipment; it’s solving real pain points for surgeons and patients alike.
Host: Let’s start with the basics. What is the QuNaMai Plasma Surgical System, and who is it for?
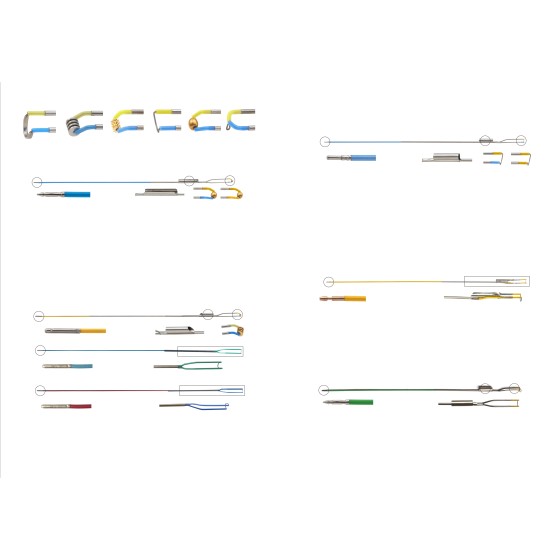
Dr. Carter: Great question! It’s an all-in-one device designed for two key specialties: urology (think prostate or bladder tumor procedures) and gynecology (specifically hysteroscopic surgeries, like endometrial treatments). Unlike single-use or single-specialty tools, this system works across both departments—so hospitals get more value from one investment. And it’s backed by QuNaMai, a brand focused on balancing precision with practicality.
Host: That cross-departmental use is a big plus. Now, what makes its technology stand out? I’ve heard it uses "low-temperature plasma"—can you explain that in simple terms?
Dr. Carter: Absolutely! Traditional electrosurgical tools use 300-400°C heat to cut tissue, which burns surrounding areas, causes scarring, and raises complication risks. This system? It operates at 40-70°C—think warm, not scalding. It uses a plasma field to break tissue molecules apart (we call it "molecular cold cutting") instead of burning. The result? Heat damage is less than 1mm deep—super shallow.
Host: Wow, that’s a huge difference. Do we have data to back up how that helps patients?
Dr. Carter: We do! A 2023 study in the Chinese Journal of Urology found this tech cuts post-op urinary incontinence risk by 62%—critical for urology patients. For gynecologists, that minimal heat means way less tissue adhesion after surgery, which lowers the chance of future fertility issues or pain. Surgeons also tell us it’s easier to control—no more worrying about accidental burns.
Host: That’s reassuring. Let me follow up—do you have real hospital cases where this system made a tangible difference? I think listeners would love to hear that.
Dr. Carter: Totally—let’s take Guangzhou Central Hospital, a busy tertiary facility that switched to this system last year. Their urology team used to do 8-10 prostate surgeries a week with traditional tools; now they’re up to 12, because the QuNaMai system cuts surgery time by 25% (from 90 mins to 65 mins on average). Even better? Post-op urinary incontinence rates dropped from 11% to 3%—right in line with that 62% reduction data.
And their gynecology department? They handle tons of hysteroscopic procedures for abnormal uterine bleeding. Before, about 15% of patients had post-op tissue adhesion; with this system, it’s down to 4%. One of their surgeons told me, “We don’t have to schedule follow-up procedures to fix adhesion anymore—that frees up my calendar and saves patients stress.” It’s those real-world wins that make this system special.
Host: That’s incredible—concrete results from a real hospital. Now, what about versatility? Does it work for different types of surgeries, even more complex ones?
Dr. Carter: It’s built for flexibility! It has two key modes: SP1 and DES. SP1 runs at 200W with 300Ω impedance—perfect for tough jobs like removing large prostates (over 80g) because it cuts through tissue efficiently without dragging. DES mode is 120W, focused on coagulation—great for gynecologists closing small blood vessels (up to 3mm) during hysteroscopies. No more switching between multiple devices mid-surgery!
Host: Safety is always top of mind for hospitals. What safeguards does this system have?
Dr. Carter: Three big ones. First, it meets CF-type anti-electrocution standards—safe to use with saline irrigation, which is common in these surgeries. Second, it eliminates TUR syndrome—you know, that dangerous condition from fluid absorption during traditional prostate surgery? This system’s design makes that risk 0%. Third, it’s compatible with patients who have pacemakers—something many older systems can’t say. For hospitals treating diverse patients, that’s a game-changer.
Host: Let’s talk practicality—hospitals care about costs and workflow too. How does this system deliver on that?
Dr. Carter: It’s a cost-saver in two key ways. First, the electrodes last 50 surgeries—industry average is 30. That means fewer replacements, less waste. Second, it uses regular saline instead of expensive specialized irrigation fluids—saves about $800 per procedure. And for workflow? 90% of patients can have their catheters removed within 24 hours (traditional surgery takes 3-5 days), and average hospital stays drop to 1.3 days. That frees up beds and lets hospitals treat more patients—like Guangzhou Central, they increased their patient throughput by 18% just from faster recoveries.
Host: Impressive. For hospitals looking to adopt this—what certifications does it have? Is it ready for global use?
Dr. Carter: It checks all the boxes. Internationally, it has ISO 13485 (medical device quality) and ISO 9001. In China, it meets GB/T 42061 and GB/T 19001 standards. It’s in stock now (SKU: BKSKU-PYDR-404) and ready for export—so hospitals worldwide can access it.
Host: Perfect—so if a hospital wants to see specs, or even book a demo, where do they go? Can we share any links for that?
Dr. Carter: Absolutely—we’ve made it easy. The best first step is visiting the official product page: that’s https://www.tl-wc.com/products/46. There, they can find full specs, high-res photos of the system, and a downloadable brochure with all the clinical data we talked about. If they want to see it in action, there’s a “Book Virtual Demo” button on that page too—our team will walk them through a live simulation of how it works in urology and gynecology cases. They can also email our procurement team directly at QuNaMai@163.com if they have pricing questions.
Host: Final question—who should be the first to reach out? Is this just for large hospitals, or smaller facilities too?
Dr. Carter: Any hospital that does urology or gynecology minimally invasive surgeries—big or small. Smaller hospitals love it because it replaces two separate devices (one for urology, one for gynecology), so they save on upfront costs. Larger facilities love the efficiency boost. Procurement teams, department heads, even surgeons who want to advocate for better tools—all are welcome to reach out.
Host: Elena, this was eye-opening. The QuNaMai system isn’t just innovative—it’s practical, safe, and patient-centered. And for listeners wanting to dive deeper, remember: the product page (https://www.tl-wc.com/products/46) has specs, demos, and contact info—all in the show notes too, so you don’t have to jot down the URL. Thanks again for joining!
Dr. Carter: Thanks for having me—here’s to safer surgeries and happier patients!
Related Products