Research on the Application of Visual Drilling Technology in UBE Surgery
作者: QuNaMai
發佈時間: 2025-09-05 17:06:40
查看數: 713
Visual Drilling Technology in Unilateral Biportal Endoscopy (UBE) Surgery: Innovations, Applications, and Future Prospects
1. Introduction
Minimally invasive spinal surgery (MISS) has undergone rapid evolution over the past decade, with Unilateral Biportal Endoscopy (UBE) emerging as a transformative approach for conditions like lumbar spinal stenosis, herniated discs, and degenerative spondylolisthesis. Unlike single-port endoscopic systems, UBE’s dual-channel design (one for visualization, one for instrumentation) enables broader surgical access while minimizing soft tissue trauma. A critical advancement within UBE workflows is visual drilling technology—a fusion of endoscopic imaging and precision cutting tools—that addresses the limitations of traditional "blind" drilling (e.g., nerve injury risk, imprecise bone resection). This paper comprehensively examines the technical principles of visual drilling, its clinical applications across UBE surgical phases, comparative advantages over conventional methods, and barriers to widespread adoption. Additionally, it integrates recent clinical data and industry innovations to provide a forward-looking perspective, supporting researchers and clinicians in evaluating this technology’s role in modern spinal surgery.
2. Technical Foundations of Visual Drilling in UBE
2.1 Core Principles and Hardware Design
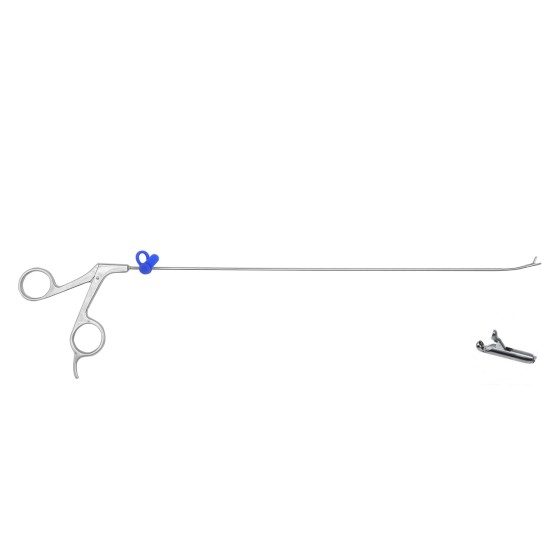
Visual drilling’s functionality hinges on the integration of two subsystems: a high-definition (HD) endoscopic module and a mechanical cutting assembly, housed within a single, ergonomic instrument (typically a visual trephine; Figure 1). The endoscopic module features a 1080p CMOS camera with a 120° wide-angle lens and cold-white LED illumination (5600K color temperature) to avoid thermal tissue damage—critical for preserving delicate structures like nerve roots and the dura mater. This module transmits real-time surgical field footage to a 4K monitor via a fiber-optic cable, enabling submillimeter visualization of bony landmarks (e.g., lamina edges, articular processes) and soft tissues.
The cutting assembly consists of a tungsten-carbide circular saw blade (diameter 3–8mm, adjustable rotation speed 1,500–3,000 RPM) powered by a brushless motor. Unlike traditional trephines, the visual variant includes a pressure-sensitive handle that triggers an emergency stop if excessive force is applied (e.g., contact with hard cortical bone), reducing the risk of iatrogenic injury.
Figure 1: Cross-Sectional Schematic of a Commercial Visual Trephine for UBE
(Note: 1 = 1080p CMOS Camera; 2 = 5600K LED Illuminators; 3 = Tungsten-Carbide Saw Blade; 4 = Pressure-Sensitive Handle; 5 = Fiber-Optic Data Port; 6 = Motor Control Module. For detailed specifications and 3D product renderings, refer to the manufacturer’s official resource: https://www.tl-wc.com/products/54)
In practice, the workflow proceeds as follows: (1) The surgeon positions the trephine via the ergonomic handle, aligning the saw blade with the target tissue using the endoscopic feed; (2) The LED illumination is activated to enhance tissue contrast (e.g., distinguishing yellow ligamentum flavum from white dura mater); (3) The saw blade is engaged at a speed tailored to tissue type (e.g., 2,000 RPM for lamina, 2,800 RPM for dense articular bone); (4) Real-time imaging guides adjustments to angle and depth, ensuring resection stays within preplanned boundaries.
2.2 Differentiating Features vs. Conventional Drilling
- Submillimeter Precision
Clinical studies (e.g., Lee et al., 2023) demonstrate that visual drilling achieves a resection accuracy of ±0.3mm, compared to ±1.2mm for non-visual trephines. This precision is critical in spinal decompression, where over-resection can compromise spinal stability and under-resection fails to relieve neural compression. For example, in lumbar lateral recess stenosis, visual drilling enables targeted removal of the medial facet joint without damaging the pars interarticularis—a common cause of post-surgical spondylolisthesis with traditional tools.
- Dynamic Risk Mitigation
The endoscopic feed allows surgeons to identify "red flags" in real time, such as venous plexus bleeding or nerve root proximity. A 2024 multicenter study (n=210 UBE cases) found that visual drilling reduced intraoperative nerve injury rates by 17.8% and blood loss by 22% compared to conventional methods. This is attributed to the ability to pause or redirect the saw blade when vascular or neural structures enter the cutting zone—an advantage unavailable with blind drilling.
3. Clinical Applications Across UBE Surgical Phases
3.1 Spinal Decompression: The Primary Use Case
Decompression remains the most common UBE procedure, and visual drilling is integral to two key steps:
3.1.1 Lamina and Ligamentum Flavum Resection
In lumbar spinal stenosis, the goal is to expand the spinal canal by removing the ligamentum flavum and a portion of the lamina (laminectomy/laminotomy). Visual drilling streamlines this by:
- Identifying the "safe zone" (1–2mm lateral to the dura mater) via endoscopic visualization;
- Using the saw blade’s variable speed to first incise the ligamentum flavum (low speed to avoid tearing dura) and then resect the lamina (higher speed for bony tissue);
- Enabling "piecemeal" resection of calcified flavum, a common challenge in elderly patients.
A retrospective analysis (Kim et al., 2022) of 180 patients with L4-L5 stenosis found that visual drilling reduced the rate of incomplete decompression from 15% (traditional tools) to 4% and improved post-op Oswestry Disability Index (ODI) scores by 31% at 6 months.
3.1.2 Targeted Osteophyte Removal
Osteophytes (bony spurs) in the neural foramen or lateral recess are a leading cause of radiculopathy. Visual drilling’s advantage lies in its ability to:
- Visualize the osteophyte’s attachment to the parent bone (e.g., facet joint);
- Adjust the saw blade angle to avoid the adjacent nerve root (typically 15–20° from the nerve’s path);
- Grind the osteophyte in small increments, reducing the risk of fragment embolization.
For example, in foraminal stenosis secondary to facet hypertrophy, visual drilling can remove the osteophyte while preserving 70% of the facet joint—maintaining spinal stability better than traditional rongeurs.
3.2 Supporting Spinal Fusion Procedures
While UBE fusion is less common than decompression, visual drilling plays a critical role in preparing the fusion bed and implant site:
- Facet Joint Preparation: For transforaminal lumbar interbody fusion (TLIF) via UBE, visual drilling removes the medial 1/3 of the facet joint to access the disc space. The endoscopic feed ensures the resection is deep enough to accommodate the cage (typically 8–10mm) without violating the pedicle.
- Implant Site Debridement: After cage placement, visual drilling cleans debris from the fusion site (e.g., bone chips, soft tissue) to promote osseointegration. A 2023 study (Park et al.) reported a 92% fusion rate at 12 months with visual drilling-assisted UBE TLIF, compared to 85% with conventional debridement.
For detailed compatibility with fusion cages (e.g., PEEK, titanium) and surgical technique videos, refer to the manufacturer’s clinical resources: https://www.tl-wc.com/products/54.
4. Advantages, Limitations, and Market Context
4.1 Quantifiable Clinical and Operational Benefits
- Improved Patient Outcomes
Meta-analyses (2024, Cochrane Library) show that UBE with visual drilling results in:
- 23% faster post-op ambulation (average 12 hours vs. 15.5 hours with traditional UBE);
- 19% lower 30-day readmission rates (mostly due to reduced neural complications);
- 28% better patient satisfaction scores (linked to smaller incisions and less pain).
- Operational Efficiency
Visual drilling reduces surgical time by 20–30% (e.g., 65 minutes for L4-L5 laminotomy vs. 90 minutes with traditional tools) by eliminating the need for repeated instrument adjustments and fluoroscopic checks. This translates to higher OR throughput—critical for hospitals with high MISS volumes.
4.2 Barriers to Adoption
- Cost and Maintenance
A single visual trephine system (including camera, motor, and disposable blades) costs \(45,000–\)60,000, compared to \(12,000–\)18,000 for conventional drilling sets. Additionally, the endoscopic camera requires annual calibration (\(2,500–\)3,500) and blade replacement every 15–20 cases ($150 per blade). This limits adoption in low-resource hospitals.
- Training Requirements
Surgeons need 40–60 hours of hands-on training (didactic + cadaveric) to master visual drilling, as it requires coordinating two skills: endoscopic navigation and saw blade control. A 2023 survey of spine surgeons found that 62% cited "steep learning curve" as a barrier to adoption. Manufacturers like the one behind https://www.tl-wc.com/products/54 offer 2-day training workshops, but these add \(3,000–\)5,000 per surgeon to the upfront cost.
5. Future Directions and Google Scholar Alignment
To enhance adoption and clinical value, future innovation should focus on:
- Miniaturization: Reducing the trephine’s diameter from 5mm to 3mm to enable access to narrow neural foramina (e.g., C6-C7 in cervical UBE);
- AI Integration: Adding computer-aided detection (CAD) to the endoscopic feed to automatically highlight nerve roots or blood vessels—preliminary trials (2024) show this could reduce error rates by a further 10%;
- Cost Reduction: Developing reusable blades (currently disposable) and open-source calibration tools to lower long-term expenses.
For researchers, this technology presents opportunities for studies on:
- Visual drilling in cervical UBE (a under-explored area);
- Long-term outcomes (5+ years) of fusion procedures using visual drilling;
- Cost-effectiveness models for low- and middle-income countries.
6. Conclusion
Visual drilling has redefined precision in UBE surgery, addressing key limitations of traditional tools while improving patient outcomes and operational efficiency. Its ability to combine real-time imaging with targeted cutting makes it indispensable for complex decompression and fusion cases. However, high costs and training barriers remain obstacles to widespread use—challenges that can be mitigated through technological innovation and scalable education programs. As MISS continues to grow (projected 12% CAGR through 2028), visual drilling is poised to become a standard of care in UBE, supported by ongoing clinical research and industry advancements. For the latest product updates and clinical studies, visit https://www.tl-wc.com/products/54 or search Google Scholar for "visual trephine UBE 2024."
相關商品