Surgical treatment classification and strategies for cervical spondylosis of nerve root type
Author: QuNaMai
Release time: 2025-09-14 19:07:45
View number: 1198
Surgical treatment classification and strategies for cervical spondylosis of the nerve root type
Cervical spondylosis of the nerve root type is a common orthopedic disease. Most patients can achieve good results through conservative treatment, while only a few patients (about 10%) require surgical intervention. Among the cases of cervical spondylosis that have undergone surgery, the majority are of the spinal cord type, while the surgical cases of the nerve root type are relatively few, resulting in a slower accumulation of clinical experience in this field.
Based on literature reviews, textbook references, lectures and personal clinical experience, surgical cases of cervical spondylosis of the nerve root type can be classified into three categories: intervertebral disc type, intervertebral foramen type and uncinate osteophytes type. The following introduces the corresponding surgical strategies and technical key points for each type.
1. Intervertebral disc type
This is the most common type, caused by intervertebral disc protrusion or prolapse (soft compression lesion) compressing the nerve root area. The treatment is relatively simple, only requiring the removal of soft compressing substances. There are two surgical options:
Anterior cervical discectomy and fusion (ACDF) : A classic surgery that involves removing a protruding intervertebral disc and implanting a fusion device to achieve decompression and cervical stability reconstruction.
Keyhole technique: A minimally invasive surgical method that creates a small channel through a tiny incision and precisely removes the protruding intervertebral disc under a microscope. It has the advantages of less trauma and faster recovery.
2. Intervertebral foramen type
The term "intervertebral foramen type" is not entirely accurate. As shown in the attached figure, this type refers to the narrowing of the intervertebral foramen caused by cervical misalignment (such as vertebral body displacement or abnormal curvature). During the operation, intervertebral dilation and spinal alignment adjustment are required. The specific steps are as follows:
First, implant screws into the lower vertebral body to establish a stable support point.
Then, screws are used to expand and reposition the upper vertebral body to correct the cervical curvature and vertebral body displacement, thereby expanding the intervertebral foramen and alleviating the compression of nerve roots.
3. Unhook osteophyte type
This type is caused by hyperplasia and osteophyte formation of the uncinate process, which compresses the nerve roots and triggers root-related symptoms such as pain, numbness, muscle weakness, and even muscle atrophy. The attached image in point 6 shows a postoperative CT scan of a typical case.
3.1 Review of Unhook Process Anatomy
Mastering local anatomy is the foundation for surgeons.
• Figure 1: Definition of hook and spike dimensions:
◦ Height (1) : The vertical distance from the tip of the uncinate process to the upper surface of the vertebral body.
◦ Width (2) : For the C5 hook process, the average height is 7.10 mm and the average width is 5.74 mm.
• Figure 2: Measurement of the width of the uncinate processes at different vertebral margins (anterior 2, middle 3, posterior 4) and the distance between the medial edges of the bilateral uncinate processes (C5 level) :
The distances between the inner edges: 18.07 mm for the front, 16.13 mm for the middle, and 14.40 mm for the rear. The hook processes converge from front to back and inward.
• Figure 3: Spatial relationship among the uncinate process, vertebral artery and nerve root (C5 level) :
Angle (1) : The Angle between the posterior tip of the uncinate process and the vertebral artery is 35.70°.
◦ Distance (2) : 1.66 mm (the vertical distance from the posterior tip of the uncinate process to the nerve root).
Distance (3) : 1.94 mm (the shortest distance from the lateral wall of the uncinate process to the vertebral artery).
• Figure 4: Distance from the uncinate process to the vertebral artery (C5 level) :
◦ Distance (1) : 5.21 mm (from the inferior medial margin of the uncinate process to the vertebral artery).
◦ Distance (2) : 3.80 mm (from the upper end of the uncinate process to the vertebral artery).
• Figure 5: Supracular space of the uncinate vertebrae (the distance from the upper end of the C5 uncinate process to the adjacent upper vertebral body) : 2.12 mm.
3.2 Decompression through unhook process resection
The first two types (intervertebral disc type and intervertebral foramen type) do not require the removal of the uncinate process; conventional decompression is sufficient. However, for the uncinate osteophyte type, resection is necessary - simple longitudinal dilation cannot relieve axial stenosis and nerve root compression. This surgical technique is relatively difficult. The steps are as follows:
1. Routine preparation of the intervertebral space: Retain the posterior longitudinal ligament (PLL) on the planned resection side (or initially retain a thin layer of the posterior longitudinal ligament).
2. Use high-speed grinding drills to remove the proliferated hook protrusions:
Remove two-thirds of the superficial layer from top to bottom.
Remove the deep one-third from the inside out.
Control the depth of resection to reduce the risk of nerve root injury, and preserve a thin layer of bone on the lateral side to protect the vertebral artery.
3. Use a nerve stripping tool or a scraper to gently break and remove any remaining uncinate bone fragments.
After the resection is completed, use Kerrison biting pliers to remove the posterior longitudinal ligament to ensure adequate decompression of the nerve root. Insert a negative pressure drainage tube that is one size larger than the usual model.
3.3 Partial excision of the unhook process
Nerve root compression caused by hyperplasia of the uncinate process usually originates from the deep part of the uncinate process, and the superficial part does not need to be removed. Theoretically, only partial resection of the deep part of the uncinoid process can achieve adequate decompression, which has two key advantages:
1. The superficial uncinate process remains intact to maintain the stability of the vertebral body.
2. As the vertebral artery is located on the outer side of the deep two-thirds of the vertebral body, partial resection of the deep part of the uncinate process reduces the risk of vertebral artery injury.
3.4 Technical Key Points of Partial resection of the unhook process
1. Surgical position and incision selection: It is best to perform the operation from the opposite side. For instance, to remove the osteophyte on the right side, make a skin incision on the left side and stand on the left side of the patient. This allows the microscope to tilt so that the origin of the nerve roots can be clearly observed.
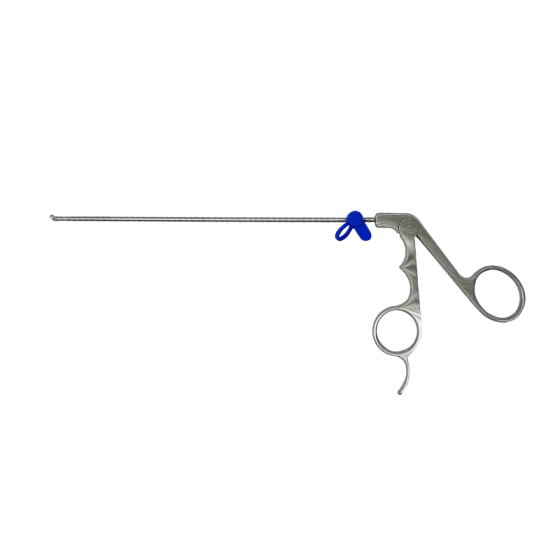
2. Use of grinding drills under a microscope: Performing surgeries under a microscope to enhance visualization and lighting effects. Compared with scrapers or biting pliers, drills cause less trauma, have higher stability, and reduce the risk of nerve damage and bleeding. The author's preferred technology
First, use a 5-millimeter "watermelon head" drill to remove most of the deep part of the hook protrusion.
Then, switch to a 3-4 millimeter diamond grinding drill for fine grinding until only a thin layer of skin (visible cracks) remains.
Finally, gently remove the remaining leather with a small hook or spatula.
3. Signs of adequate decompression:
There is no resistance when using a hook to explore the area around the nerve root.
The hook can reach the pedicle of the lower vertebral body.
The origin of the nerve roots can be directly seen under a microscope.
Clinical case examples
Recently, there was a patient who was unable to raise his shoulder within 10 days, and his deltoid muscle strength was grade 2. Two days after partial resection of the uncinate process, the patient regained the function of raising the shoulder and the deltoid muscle strength improved to grade 4. The treatment effect is very satisfactory.
4. Should uncleidectomy be performed for cervical spondylosis of the nerve root type?
It is unscientific to generally say whether uncinectomy is necessary or not, as these three types are significantly different:
The incidence of intervertebral disc type is the highest, accounting for the majority of surgical cases.
Unhook osteophyte type is relatively rare and has a low proportion of cases.
Surgeons should:
• Study textbooks, literature and attend lectures.
Understand statistical knowledge.
Engage in independent thinking and objective analysis.
The surgical treatment of cervical spondylosis of the nerve root type requires decision-making based on classification, critical thinking and flexibility. There is no one-size-fits-all solution to all cases.
Related Products